1. Inadequate Care and Facilities
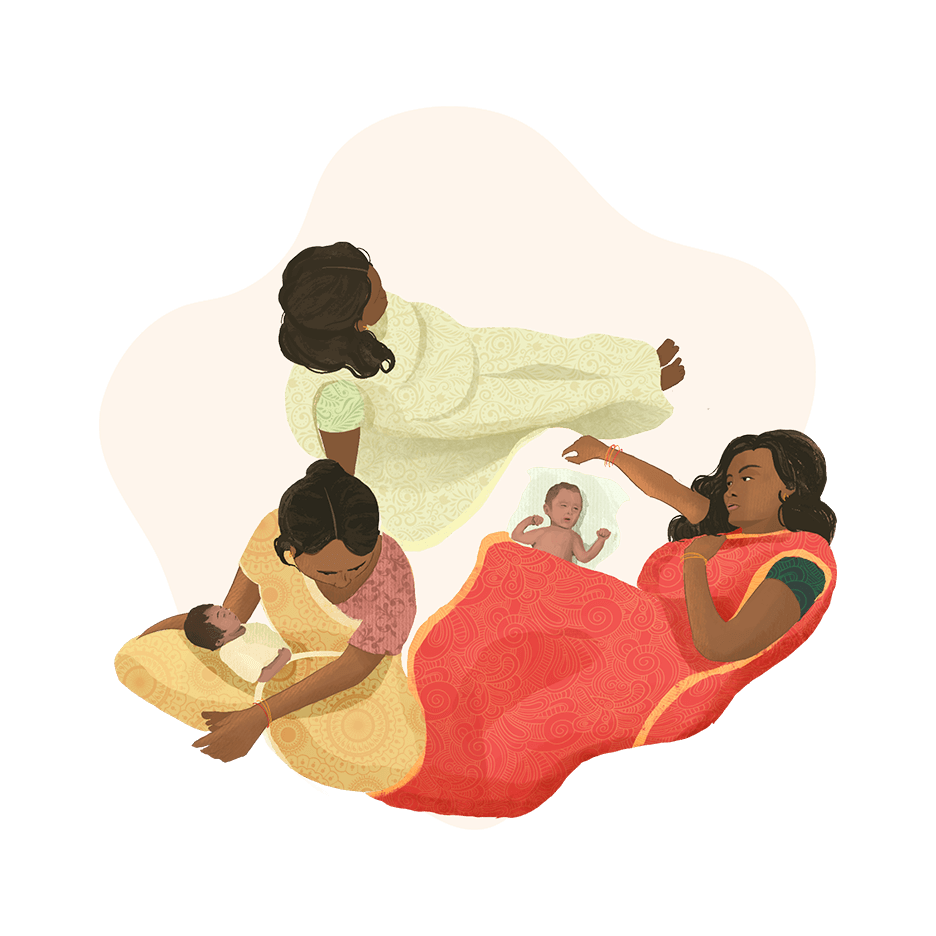
“Too Little, Too Late” refers to care that is inadequate or delayed, due to insufficient access to well-trained healthcare providers, poor infrastructure, unreliable medicine availability, and a weak referral system.
“Too Little, Too Late” remains widespread, resulting in:
Maternal mortality rate
Pregnancy to 42 days after birthXThe annual number of female deaths from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes) during pregnancy and childbirth or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy.
SRS, Sample Registration System, Office of the Registrar General, India. 2022. “Special Bulletin on Maternal Mortality in India 2018-2020.” Accessed 4 Jan 2023. https://censusindia.gov.in/nada/index.php/catalog/44379/download/48052/SRS_MMR_Bulletin_2018_2020.pdf
per 100,000 live births
in 2018-2020
UN, United Nations. “Ensure healthy lives and promote well-being for all at all ages: Targets and Indicators” Accessed on 4th Jan 2023. https://sdgs.un.org/goals/goal3
Sustainable Development Goal Target 3.1 for 2030
Neonatal mortality rate
Within the first 28 days after birth
MoHFW, Ministry of Health and Family Welfare, Government of India. 2021. “National Family Health Survey (NFHS-5) 2019-2021. Compendium of Fact Sheets: Key Indicators India and 14 States/UTs (Phase-II).” https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
per 1,000 live births
in 2019-2020
UN, United Nations. “Ensure healthy lives and promote well-being for all at all ages: Targets and Indicators” Accessed on 4th Jan 2023. https://sdgs.un.org/goals/goal3
Sustainable Development Goal Target 3.2.2 for 2030
Infant mortality rate
Within the first year after birth
MoHFW, Ministry of Health and Family Welfare, Government of India. 2021. “National Family Health Survey (NFHS-5) 2019-2021. Compendium of Fact Sheets: Key Indicators India and 14 States/UTs (Phase-II).” https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
per 1,000 live births
in 2019-2020
Under-five mortality rate
Within the first 5 years after birth
MoHFW, Ministry of Health and Family Welfare, Government of India. 2021. “National Family Health Survey (NFHS-5) 2019-2021. Compendium of Fact Sheets: Key Indicators India and 14 States/UTs (Phase-II).” https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
per 1,000 live births
in 2019-2020
UN, United Nations. “Ensure healthy lives and promote well-being for all at all ages: Targets and Indicators” Accessed on 4th Jan 2023. https://sdgs.un.org/goals/goal3
Sustainable Development Goal Target 3.2.1 for 2030
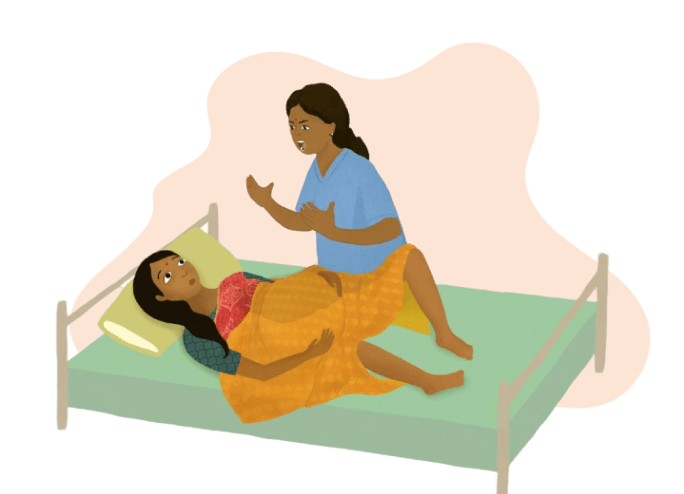
2. Excessive Medical Intervention
“Too Much, Too Soon” refers to the routine over-medicalisation of pregnancy and childbirth by the unnecessary use of non-evidence-based interventions or the use of interventions that can be life-saving when used appropriately, but harmful when applied routinely or overused.
C-sections, inductions, augmentations, and episiotomy rates are much higher than recommended in most parts of India.
Caesarean Epidemic
Across India
Private sector
MoHFW, Ministry of Health and Family Welfare, Government of India. 2021. “National Family Health Survey (NFHS-5) 2019-2021. Compendium of Fact Sheets: Key Indicators India and 14 States/UTs (Phase-II).” https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
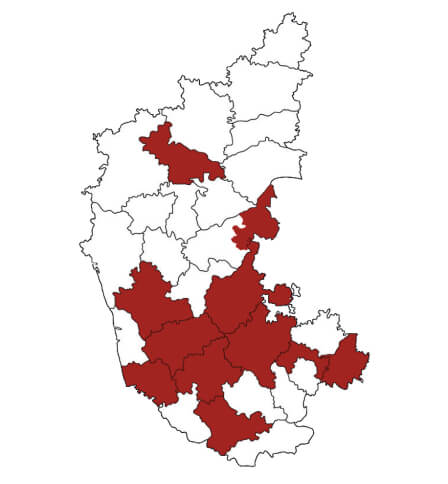
Karnataka
Private sector
MoHFW, Ministry of Health and Family Welfare, Government of India. 2021. “National Family Health Survey (NFHS-5) 2019-2021. Compendium of Fact Sheets: Key Indicators India and 14 States/UTs (Phase-II).” https://main.mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf
Caesarean Epidemic
Private Hospitals - Karnataka
Telangana
State-wide
IIPS, International Institute for Population Sciences. 2020. “Fact Sheets: Key Indicators, National Family Health Survey (NFHS-5) 2019-2020.” https://rchiips.org/NFHS/NFHS-5_FCTS/NFHS-5%20State%20Factsheet%20Compendium_Phase-I.pdf
J&K, Telangana & WB
Private sector
IIPS, International Institute for Population Sciences. 2020. “Fact Sheets: Key Indicators, National Family Health Survey (NFHS-5) 2019-2020.” https://rchiips.org/NFHS/NFHS-5_FCTS/NFHS-5%20State%20Factsheet%20Compendium_Phase-I.pdf
All data as per NHFS – 5 (2019-2020)*
v/sBoerma, Ties, Carine Ronsmans, Dessalegn Y Melesse, Aluisio J D Barros, Fernando C Barros, Liang Juan, Ann-Beth Moller, et al. 2018. “Global epidemiology of use of and disparities in caesarean sections.” The Lancet 392 (10155): 1341–48. https://doi.org/10.1016/S0140-6736(18)31928-7. – Molina, George, Thomas G. Weiser, Stuart R. Lipsitz, Micaela M. Esquivel, Tarsicio Uribe-Leitz, Tej Azad, Neel Shah, et al. 2015. “Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality.” JAMA 314 (21): 2263. https://doi.org/10.1001/jama.2015.15553.
Ideal population-level caesarean rates
Episiotomies
In India, episiotomies are the norm and are cut for
Singh, Shalini, Tushita Thakur, Nomita Chandhiok, and Balwan Singh Dhillon. 2016. “Pattern of episiotomy use & its immediate complications among vaginal deliveries in 18 tertiary care hospitals in India.” Indian Journal of Medical Research 143 (4): 474–80. https://doi.org/10.4103/0971-5916.184304.
of first time mothers, as per a study in 18 tertiary care Indian hospitals.
This is despite WHO guidelines, which recommend that episiotomies are restricted and used only when medically needed.
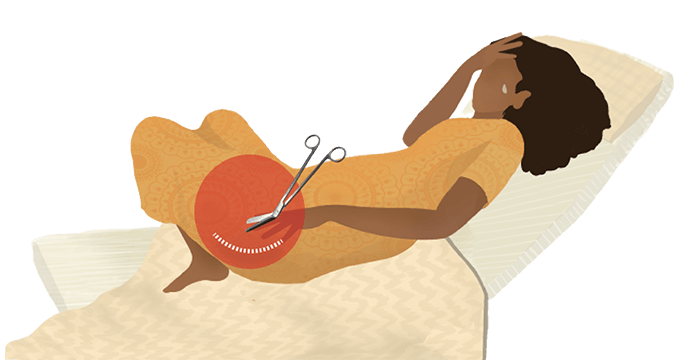
A restricted episiotomy policy results in 30% fewer women with severe perineal trauma.
3. Widely Prevalent Disrespect and Abuse
Labouring mothers experiencing physical and verbal abuse, discrimination and coercion, non-consented care, lack of privacy, and lack of confidentiality is an inherent violation of human rights and is widely prevalent in India.
Disrespect during maternity inflicts trauma on birthing mothers and reduces women’s willingness to seek medical help.
4. Lack of Demand for High Quality Care
Poor awareness, low expectations, and a lack of choice and agency accorded to expectant mothers has led to suboptimal care becoming the norm.
Families are conditioned to not expect or demand high quality care. This leads to minimal pressure on healthcare facilities to improve.